When ‘Thank You for Your Service’ Is No Longer Enough:
Special Forces, PTSD & bTBI
*George Lindenfeld, Ph.D., A.B.P.P. Reset Therapy Professional Institute,Arden, NC.
Terry Zumwalt, M.D. Operation Firehawk, PLLC
George Rozelle, Ph.D., QEEG-D, MindSpa, Sarasota, FL
Katherine Billiot, Psy.D., BCB, BCN Medical Psychology Center, Ormond Beach, FL
John Hummer, Ph.D., BCN. Frontier Health – Holston Counseling Center, Kingsport, TN
*Corresponding Author: George Lindenfeld, Ph.D.; Mailing Address: 7 Holiday Drive, Arden, N.C. 28704. E-mail: [email protected]
Abstract: The Defense and Veterans Brain Injury Center notes that since the year 2000, over 383,947 cases of military-incurred incidents of TBI have been reported. Roughly 50% of the above number concurrently experience PTSD as well as sleep disorder and other comorbid conditions. One-third also experience depression that may include suicidal ideation and attempts. Estimated disability compensation for service-connected claims is projected at 20.28 billion per year, exceeding 515 billion dollars in the next 50 years. Both PTSD and bTBI/TBI have neuro-inflammatory aspects that create brain cellular damage thought to lead to cellular aging. There is no current evidence-based treatment available that addresses these conditions. Increasing scientific support is available for the perspective that Photo-biomodulation stimulates the production of cellular energy in damaged tissue as well as enhancing the inter-connectivity between cells. A case study is provided wherein Photo-biomodulation was provided to a veteran (Dwayne W.) with multiple concussive experiences. His quantitative electroencephalograph (qEEG) results revealed a statistical and clinically significant decline in his TBI Severity Index score following three months of near infrared light (NIR), treatment. His subjective comments noted an improvement in his attentional and short and long-term memory abilities.
Keywords: blast Traumatic Brain Injury (bTBI); multiple concussions; Photo-biomodulation; Near infra-red light (NIR); loss of consciousness (LOC).
Public Significance Statement
Near infra-red light is demonstrating efficacy in the repair of cellular brain tissue damaged through concussion-related or blast-incurred injury. Special Operation Forces are particularly vulnerable to impact of this kind. A scientifically validated treatment for head injury is greatly needed to enhance the quality of life for afflicted military and civilians and their caretakers. Near infra-red light may hold the remedial key.
Introduction
The Centers for Disease Control and Prevention define a traumatic brain injury (TBI) as,“a disruption in the normal function of the brain that can be caused by a bump, blow, or jolt to the head, or penetrating head injury” (“Traumatic Brain Injury | Concussion | Traumatic Brain Injury | CDC Injury Center,” 2019, para 2). Those who serve in combat face an additional element consisting of proximity to explosive blast shockwaves. Among those diagnosed, it is estimated that upwards of 28% of this group have been exposed to multiple incidents of traumatic brain injury (mTBI) and have co-occurring PTSD (Naeser et al., 2019). Furthermore, it is estimated that 60% of injuries among military personnel who served in Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF), were due to blast-incurred explosions related to improvised explosive devices (IED’s) (Ling, Bandak, Armonda, Grant, & Ecklund, 2009).
Combat detailed service members are repeatedly exposed to blast overpressure when firing heavy weapons, such as “anti-tank recoilless rifles or heavy caliber (.50) rifles. (Fish & Scharre, 2018, p 5). The primary effects of blast exposure are best understood as related to visual, auditory, and respiratory mechanisms. The energy emanating from the explosive impact on the body is altered into dynamic energy that can damage the body and brain due to pressure waves. “Compared to controls, veterans with mTBI (with or without PTSD) exhibited … subtle impairments in verbal fluency, cognitive processing speed, attention, and working memory, similar to those reported in the literature for patients with cerebellar lesions” (Peskind et al., 2011, para 1).
A five-year follow-up study of service members who had experienced bTBI compared with combat-veteran controls free of exposure to bTBI revealed a worsening of outcome measures among the bTBI involved personnel. Cognitive factors surprisingly weren’t differentiated between the two groups; however, both PTSD and depressive symptomology appeared to be significantly elevated. Additionally, anxiety levels and sleep disturbance were also prominent in comparison to the control group.
“… this group of service members with non-medically evacuated concussion was found to have a much greater level of global disability than previously reported in prospective studies of comparable civilian patients with mild TBI, even those with multisystem trauma. This has important implications for the translatability of these combined concussive blast findings because there are far greater numbers of service members who sustain concussion exposures in combat that are not medically evacuated” (Donald et al., 2019).
A ten-year longitudinal study of civilian TBI patients found a 60 percent consistent level of disturbance in behavioral, emotional, and cognitive functioning across all time points in the research. Within the cognitive domain, difficulties with word-finding, cognitive-fatigue, memory and the sustaining of attention remained constant issues over time. The presence of irritability remained a persistent problem for two out of three of the study participants. Less than half were able to sustain ongoing employment, and around one-third noted interpersonal relationship difficulties. “Overall, problems that were evident at two years post-injury persisted until 10 years post-injury” (Ponsford et al., 2014).
The above disparate groups reveal a consistency of issues that manifest over a five to a ten-year period of time. Comparatively, the bTBI members appear to have sustained a greater level of disability although both groups have cognitively related issues including disturbance in executive functioning. Seemingly, impact to the brain has ongoing deleterious effects for a preponderance of those affected by this experience.
Since the year 2000, over 383,947 military-related incidents of TBI have been reported by the Defense and Veterans Brain Injury Center (“DoD Worldwide Numbers for TBI,” 2018). A recent experimental study involving laboratory animals investigated the effects of cumulative (three) concussive injuries as compared to a singular event in young adult male rats. Seven to eight weeks post-injury, the animals were evaluated through multimodal MRI procedure to compare both cognitive and motor deficits.
Rats hit one time revealed restricted injury to the central amygdala and caudate/putamen. Those animals struck three times evidenced diffusivity and hypo-functional connectivity in ‘white matter tracts, basal ganglia, central amygdala, brainstem, and cerebellum. Comparing three hits to one hit showed a similar pattern of change underscoring a dose effect of repeated head injury on the brainstem and cerebellum” (Kulkarni et al., 2019, para 3).
In VA facilities, 80% of veterans diagnosed with TBI also experience comorbid conditions, with roughly 50% also diagnosed with PTSD. White matter brain tissue degeneration and inflammation may take place years after a sole incident of injury to the brain. The most commonly reported difficulties among those with the condition are attentional and concentration matters. Additional consequences associated with mTBI in veterans include cognitive impairment, alcohol misuse and binge drinking, pain disorders, interpersonal conflict, and unemployment (Naeser et al., 2019)
In veterans, the majority of mTBIs that have been sustained fall into the mild category (Stocker et al., 2014). However, it is estimated that sleep disturbances are present in 30 to 70% of this impaired population. Insomnia, hypersomnia, nightmares, and irregular sleep/wake patterns following an mTBI event have been shown to impede cognitive and neurological functioning (Stocker et al., 2014).
Co-occurrence Of bTBI and PTSD
The association between the residual effects of mTBI among SOF personnel and the co-occurring PTSD diagnosis remains uncertain. Researchers have found an association between veterans with repeated incidents of bTBI and chronic PTSD (Kontos et al., 2012). The primary brain-related pathology associated with mTBI is that of traumatic axonal injury, which has been found in post-mortem cortical tissue. In contrast, gray matter change in the brain is primarily associated with PTSD.
Explicit memory (consciously recalled) and implicit memory (typically involving unconscious processes) are known to involve different neural pathways. Bodily memories may become dissociated from discrete events, especially when components of the traumatic memory are stored in a fragmented, unprocessed and temporally unbound form. In a recently submitted article (Author et al., 2019d) we discussed research regarding the issue of cellular memory. We postulated that a ‘perimeter warning barrier’ becomes created in ‘memory’ microtubules on the involved external muscle cell membrane (Lipton, 2012). Inquiry into this muscle trauma memory phenomenon may further help to clarify how those service members who experience loss of consciousness may also develop concurrent PTSD.
Shared features of bTBI and PTSD include an inflammatory aspect and glutamate excitotoxicity factor via excessive availability in the extracellular space surrounding nerve cells, which can result in cellular damage. In combination, both components may aggravate brain functioning through unmodulated over-activity (Kaplan et al., 2017). Researchers are investigating the long-term effects of these dual conditions, including the aging process. As Hayes (2019, p 4) has noted, “… there is initial evidence that these disorders accelerate brain and cellular aging.
Moreover, accumulating evidence has identified an association of these conditions with risk of later development of neurodegenerative disease, as both mTBI and PTSD have been linked with increased risk for Alzheimer’s disease. Furthermore, C-reactive protein – a biomarker for the presence of neuro-inflammation – has also been found to be elevated in both TBI and PTSD. The presence of this protein raises the likelihood of enduring and “persistent post-concussive symptoms, cognitive impairment, and ongoing psychological issues 3 months after mTBI” (Romeu-Mejia, Giza, & Goldman, 2019, para 24).
Recent investigators have focused on the resting-state brain neural network, referred to as the default mode network (DMN), a measure of the degree of functional connectivity of the brain (Santhanam, Wilson, Oakes, & Weaver, 2019.) The study compared veterans with dual diagnoses (PTSD/mTBI) to service members with only mTBI. As noted by the study authors, “For all subjects with mTBI, default network connectivity correlated inversely with PTSD checklist score (p < 0.05). Additionally, distinct associations (p < 0.05) between medial prefrontal cortex connectivity and PTSD symptoms. Posterior cingulate cortex connectivity and mTBI-related cognitive deficits were also significantly related.” (Santhanam, Wilson, Oakes, & Weaver, 2019, para 1.)
Another recent study explored self-report health outcome measures in an mTBI/PTSD group as compared to an mTBI group and healthy control (HC) group. The most negative health outcomes were reported by the mixed mTBI/PTSD group. “Individuals in either mTBI group performed worse than those in the HC on verbal learning and memory and psychomotor speed. Health outcomes were correlated with mental health and post-concussive symptoms, as well as neuropsychological variables” (Bomyea et al., 2019, para 1)
Personal and Familial Impact
Spouses of the injured veteran with either PTSD/bTBI or both “experience tremendous emotional, financial, and social challenges that arise from being the caregiver for their husbands—feel isolated from and abandoned by both the military community and the civilian community” (Voris & Steinkopf, 2019, para 1). Furthermore, the stresses they confront in daily life are amplified by the social and emotional disconnection these women experience.
Another study reported that the caretaker of those with PTSD/bTBI spent the majority of their time providing emotional support and dealing with behavioral problems (Casler, 2019). The caregiver’s reported forgetfulness and anxiety as being severe. Many caregivers themselves demonstrated clinical levels of anxiety and/or major depression. Poorer heart health was correlated with higher scores for depressive symptoms and perceived stress in these caregivers.
A final reference in this section pertains to the status of children who have an injured military parent. Hisle-Gorman, Susi, & Gorman (2019) hypothesized that military parental injury would negatively impact the preventive care, injuries, rates of maltreatment, mental health care, and need for psychiatric medication prescriptions of military children. They tracked doctor visits and prescription data of over 485,000 military-related children ranging from two years of age to sixteen. Decreased rates of preventive care visits; increased rates of visits for injuries, maltreatment, and mental health care; and increased psychiatric medication use were noted for children of injured military parents. More pronounced changes across all categories of care were noted for children of parents with posttraumatic stress disorder (PTSD).
Cost Factors
A national study in 2012 of US OEF/OIF veterans receiving treatment through the VA for TBI estimated their healthcare service costs to be fourfold, compared to those of non-TBI patients ($5,831 vs. $1,547). When PTSD was added to the mix, a median cost of $5,053 per capita was indicated (Taylor et al., 2012). On an annual basis, the estimated cost of healthcare for veterans with comorbid TBI-depression is more than $1 billion. (Dismuke-Greer et al., 2019). Damage to visual functioning alone among those with TBI annually is estimated at $2.4 billion (Frick & Singman, 2019).
Estimated disability compensation for service-connected claims is projected at $20.28 billion per year, anticipated to 515 billion dollars in the next 50 years. The total projected VA inpatient and outpatient costs are estimated at “3.63 billion dollars and $1.48 billion annually, and this represents $106.4 billion and 40.4 billion over the next 50 years, respectively” (Thakur et al., 2018). Cushman (2012) found that in a poly-trauma group, just as in the general Veterans Health Administration population, therapies for PTSD and TBA accounted for 60 percent of total health care costs (Cushman 2012).
Long-Term Neurodegenerative Complications
“Gaps in the knowledge base are still abundant, and concerns have been raised through fledgling research of an increased risk of late-life neurodegeneration after exposure to multiple TBIs; a condition termed chronic traumatic encephalopathy” (Eapen & Subbarao, 2019, para 1). Animal bTBI studies revealed the emergence of “increased anxiety, acoustic startle, and cued fear responses compared with controls… These behavioral abnormalities were also accompanied by changes in stathmin 1, a microtubule-associated protein highly expressed in the amygdala that plays a role in learning and fear responses“ (Agoston et al., 2017, p S-11).
The risk of later development of progressive neurodegenerative conditions, such as Alzheimer’s Disease (AD), is also an emerging area of study concerning veterans who experience bTBI/PTSD (Mohamed et al., 2019, para 3). Widespread accumulation of tau protein anomalies across all combinations of PTSD/TB groups “was positively correlated with neuropsychological deficit scores in the TBI+PTSD and PTSD groups” when compared to a healthy control group.”
Additionally, the deteriorative trio of oxidative damage, excitotoxicity, and neuro-inflammation are found in both conditions. “These disturbances produce neuronal death and degeneration, axonal injury, and dendritic spine dysregulation and changes in neuronal morphology (Kaplan et al., 2017, para 1). We conclude this section with a comment from the following authors, “Gaps in the knowledge base are still abundant, and concerns have been raised through fledgling research of an increased risk of late-life neurodegeneration after exposure to multiple TBIs; a condition termed chronic traumatic encephalopathy” (Eapen & Subbarao, 2019, para 1).
When neuro-inflammatory responses become chronic, the beginning and advancement of Alzheimer’s disease (AD) appears to follow. Kempuraj et al., (2019, para 1) hypothesize that “neuro-inflammatory responses resulting from mast cell activation along with the accompanying risk factors such as age, gender, food habits, emotional status, stress, allergic tendency, chronic inflammatory diseases, and certain drugs can accelerate brain injury-associated neuro-inflammation, neurodegeneration, and AD pathogenesis.
Thus, the association between PTSD/bTBI/TBI and the emergence of chronic levels of neuro-inflammation may be a precursor to the development of dementing disorders such as Alzheimer’s Disease. “TBI is also a risk factor for the development of neurodegenerative diseases including chronic traumatic encephalopathy (CTE) and Alzheimer’s disease” (Elder, Ehrlich, & Gandy, 2019, para 1).
Treatment Options
It is generally accepted that no current evidence-based interventions are available for persons suffering from mTBI/TBI (Bergersen, Halvorsen, Tryti, Taylor, & Olsen, 2017). However, a promising intervention called near-infrared (NIR) light therapy offers the possibility for remediation of some of the deleterious effects of mTBI/TBI by regenerating and repairing brain tissue. When damaged cells receive adequate near-infrared (NIR) light, it is thought that nitric oxide is released, thereby facilitating blood flow to the impaired areas. Furthermore, it appears that NIR light stimulates the production of adenosine triphosphate (ATP), which energizes mitochondrion in afflicted cells as well as enhancing the inter-connectivity between cells (Fox & Campbell, 2019).
It is well-recognized that ATP is the primary source of energy within the mitochondria of a cell. Unfortunately, behavioral and cognitive treatment interventions are unable to address executive-level cognitive damage and instead focus on strengthening remaining abilities. “Effective treatments to improve cognition in individuals with TBI are currently lacking, and these are urgently needed for veterans, as well as nonveterans. Transcranial red/NIR PBMT is a promising clinical research method to fill these needs” (Naeser et al., 2019, p 312).
Brain-derived neurotrophic factor contributes to neuronal growth and survival, facilitating the differentiation, maturation, and maintenance of cellular material. It serves as a neurotransmitter modulator and participates in neuronal plasticity, which is essential for learning and memory…Decreased levels of BDNF are associated with neurodegenerative diseases with neuronal loss, such as Parkinson’s disease, Alzheimer’s disease, multiple sclerosis and Huntington’s disease. Thus, BDNF may be useful in the prevention and management of several diseases including diabetes mellitus (Bathina, Undurti, 2015, para 1).
Inflammatory effects are deleterious particularly when they become chronic. Pharmaceutical means have been the primary intervention through the use of nonsteroidal anti-inflammatory medications. It has been found the Photo-biomodulation can accomplish the same objective without pharmaceuticals. In particular, inflammation of neurons in the brain referred to as neuro-inflammation, is particularly associated with the function of microglia that are found in the immune defense system — cells of this type hunt for plaque as well as infectious elements. In essence, their role is to sustain cellular homeostasis (Hamblin M. R., 2019).
Case Example
Dwayne W. is a 43-year-old veteran who had been involved in a service-related vehicle roll-over incident. He volunteered to participate in the present case study. The accident resulted in a brief loss of consciousness. In his youth, he had engaged in contact sports that resulted in several concussive experiences. He developed PTSD during his service in Bosnia, consequent from witnessing the results of ethnic cleansing from Serb atrocities.
Emotionally, he internalized his anger, which ultimately progressed into road rage and paranoia. At one point, he was involuntarily hospitalized in a VA psychiatric unit due to his dual PTSD/TBI conditions. His spouse became his caretaker as he was unable to function independently. Dwayne W. volunteered to participate in a pilot study involving an experimental treatment for PTSD called RESET therapy (Author et al., 2019a, b, c), experiencing full PTSD symptom remission within four brief treatment sessions.
His first awareness of positive change was that of significant sleep improvement. His behavioral improvements posttreatment were significant. He was able to engage in social activities with his family. He then increased his level of social engagement through interactions with individuals in the local veteran community. His road rage dissolved as did his paranoid tendencies. However, post-treatment assessment revealed continuing cognitive impairment involving attention, short-term memory, and long-term memory.
To seek to address his ongoing cognitive symptoms, Dwayne W. was treated with iLED light with the understanding that this was an experimental treatment. Both he and his wife signed a consent form approving the intervention, prior to engaging in the intervention. The infrared light stimulus used in this case study was the iLED component (intranasal diode) only of the Vielight Neuro Alpha headset, produced by Vielight, Inc. of Toronto Canada (www.vielight.com). The iLED diode generates near-infrared light (NIR) at a frequency of 810 nanometers, and is pulsed 10 times per second (10 Hz).
Prior to the start of the intranasally-generated near-infrared light therapy, a baseline Quantitative EEG (qEEG) was acquired in the eyes-closed condition. Neuroguide computer software (Applied Neuroscience International) was used to remove artifacts and to transform raw EEG data into quantified qEEG data. For the purposes of the present study, only the Trauma Severity Index discriminant functional analysis statistic was utilized, pre-intervention and post-intervention to measure interval change (see below).
Each day at the same approximate time of day, the intranasal diode (iLED) was first clipped onto the left nostril, and pulsed near infrared light (810 nanometer, pulsed at 10Hz) was delivered to the brain for 25 continuous minutes. The intranasal diode was then clipped onto the right nostril, and the process repeated for another 25 continuous minutes. This resulted in 50 minutes of cumulative exposure of pulsed near-infrared light per day. Dwayne performed this daily treatment regimen for seven days per week, for three consecutive months. An approximate estimate of cumulative total of light exposure = 90 days x 50 min. = 4500 minutes, divided by 60 = 75 total hours of intra-nasally-delivered pulsed near-infrared light exposure.
The specified wavelength (810 NM) enables photonic transmission through the intranasal channel to the deep ventral brain areas. The light illuminates blood circulating through the nasal region, which then circulates throughout the body. No known contraindications or major side effects have been found with iLED application, though M. Hamblin, MD has cautioned that there is an optimal level of exposure that facilitates beneficial effects, and exceeding that optimal level can potentially negate the therapeutic effects of the intervention (in the case of NIR, more light exposure is not ‘better’; optimal effects are obtained using the amount of exposure recommended by experts in the field, and by the Vielight company with respect to use of the intranasal device. The use of intranasal light therapy is endorsed by an increasing body of scientific evidence (Chao, 2019; Salehpour, Hamblin, & DiDuro, 2019; Zomorrodi, Loheswaran, Pushparaj, & Lim, 2019), presumably because the intranasal positioning permits light to be accessed by lower brain structures with connections to higher brain structures.
As noted previously Quantitative Electroencephalogram (QEEG) data were obtained to compare pre and posttreatment outcomes. Dwayne’s pre and post-photo-biomodulation treatment results are presented below (the ‘Trauma Severity Index or TSI represents a discriminant function analysis of the qEEG eyes-closed data.). The timespan between pretreatment and post-treatment TSI measures was approximately 3 months. Figure 1 depicts Dwayne’s pretreatment TSI score and Figure 2 depicts Dwayne’s post-treatment TSI score, as displayed below.
Figure 1. Traumatic Brain Injury Pre-nIR.
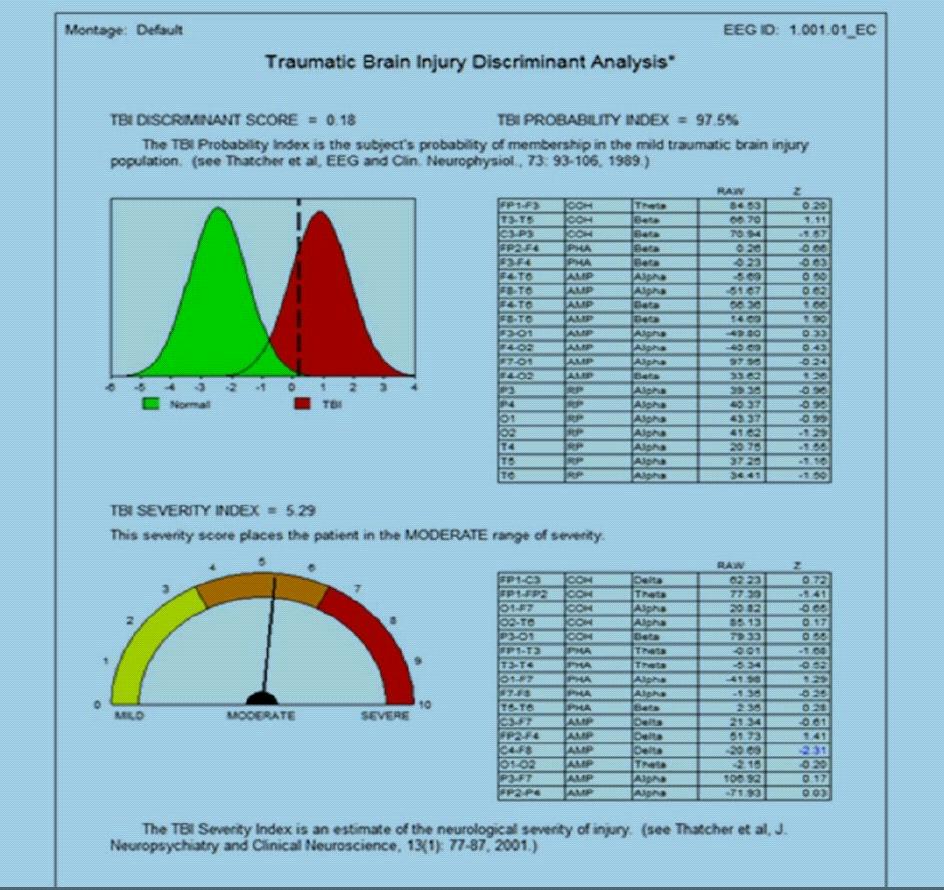
In Figure 1, the pre-treatment TBI Probability Index suggests a 97.5% statistical likelihood that the TBI Discriminant score and the TBI Severity Index represent a true finding (as opposed to a chance finding) as derived from Dwayne’s eyes-closed qEEG data set ( (Applied Neuroscience International, n.d.) His TBI Severity Index Score of 5.29 predicts that Dwayne’s TBI severity level falls within the Moderate range of functional impairment.
Figure 2. Traumatic Brain Injury Post nIR.
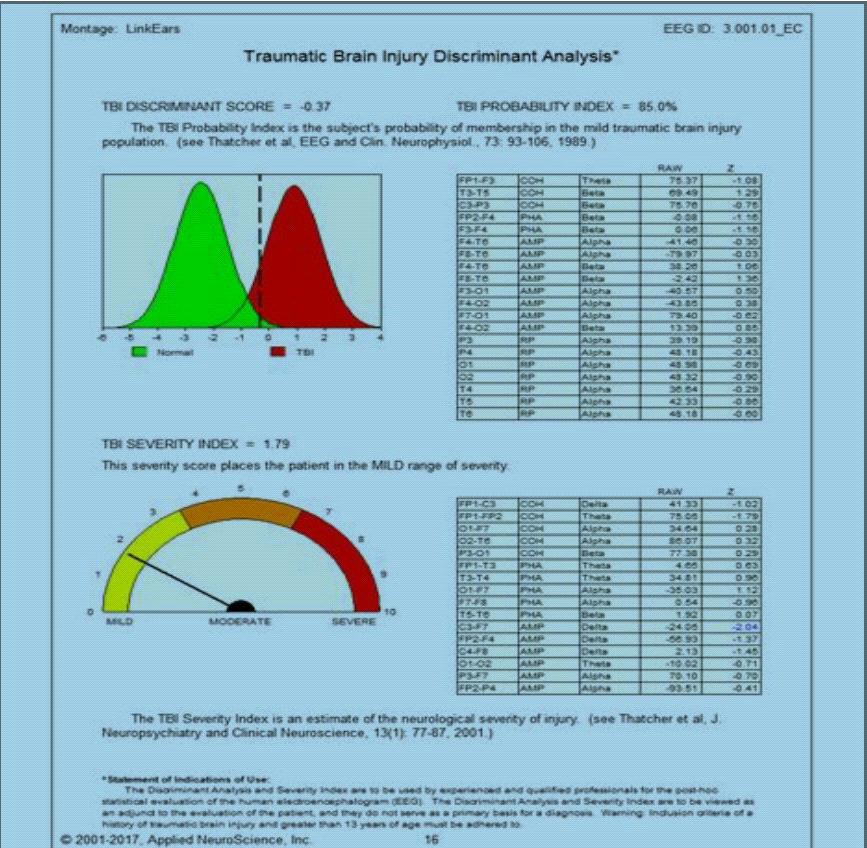
As evident in Figure 2, following three continuous months of Near-infrared (nIR) treatment, it is highly probable (85% statistical likihood) that Dwayne’s overall TBI functional severity level has now reduced from a previous Moderate degree of impairment to a current Mild degree of impairment (post-treatment TBI Severity Index = 1.79.) Rather impressively, this volunteer’s post-treatment TBI Severity Index score estimates a 67% overall reduction in TBI severity from pretreatment to posttreatment. The data pattern suggests that following a three month regimen of near-infrared light therapy exposure carefully directed at the lower brain, statistical estimates of the likelihood and severity of impairment associated with TBI have have moved in the direction of normalization.
After treatment, Dwayne reported the following: “With short-term memory matters, previously I had four little units that, when I pressed them, they would activate some location that would be revealed on my phone through an app, such as my keys. Within the last three to four weeks, I haven’t had to use the memory device at all. With long-term memory, it seems like I can retain information for a longer period of time. It hasn’t been necessary for others to remind me of things like dental appointments that are scheduled in the future. Additionally, my patience seems to have increased, particularly with my kids. My driving has improved. I’ve come to realize that I don’t always need to be driving at around 90 mph. I can’t think of any particular recent incident where someone cut me off and me becoming emotional about it like I did in the past. Overall, this light stuff is amazing.” (Dwayne W., personal correspondence 3/23/18).
Summary
Although the use of Photo-biomodulation is still in its developmental stage, research is emerging, supporting the likelihood of increased cellular activation/metabolism. “The proposed mechanism of PBM is largely assumed to involve stimulation of the cellular energy metabolism and energy production mediated by mitochondria acting as the primary cellular photoreceptor or target for absorbing the photons” (Huang & Hamblin, 2019. p 35). A second significant factor appears to be a decrease in inflammation levels forthcoming from the exposure of damaged tissue to select red/NIR wavelengths. Major implications from this finding are related to the onset of neurodegenerative conditions later in life (Hamblin, 2019). An improvement in sleep duration, executive functioning, and verbal memory has been reported in a recent study through iLED treatment (Naeser et al., 2019).
The process through which neurons are newly developed in the brain is referred to as Neurogenesis. “Neurogenesis persists in the adult mammalian brain, where it can be stimulated by physiological factors, such as growth factors and environmental enrichment, and by pathological processes, including ischemia” (Naeser et al., 2019, p 321). Additionally, Photo-biomodulation is thought to form synaptic interfaces between neurons in the brain in a Process referred to as synaptogenesis. The intervention is also showing a significant antidepressant and anti-anxiety effect (Caldieraro & Cassano, 2019).
Our case study volunteer exemplifies the Photo-biomodulation process. His therapeutic experience transformed him as an individual from the status of a high level of dependency upon others to the status of full independence, including the assumption of a leadership position in a local veteran’s community organization. He was able to reengage successfully in employment thereby contributing to the well- being of his family and to society. His spousal relationship improved dramatically as did his relationship with his children.
With the availability of future financial support, it is our hope to obtain larger volunteer samples and include random assignment to an active treatment condition (infrared light frequencies identified in previous research as most efficacious in improving residual effects of TBI), versus a sham control treatment (near-infrared light frequencies that have not proven to have therapeutic effects upon sequelae of TBI). Although the present case example involves only one individual, if we can multiply this finding by many, hope becomes available to those whose lives have been filled with despair. Those who have served deserve no less.
References
Agoston, D., Arun, P., Bellgowan, P., Broglio, S., Cantu, R., Cook, D., … Smith, D. (2017). Military Blast Injury and Chronic Neurodegeneration: Research Presentations from the 2015 International State-of-the-Science Meeting. Journal of Neurotrauma, 34(S1), S-6.
https://doi.org/10.1089/neu.2017.5220
Applied Neuroscience International (n.d.) https://appliedneuroscience.com/
Alway, Y., McKay, A., Gould, K. R., Johnston, L., & Ponsford, J. (2016). Factors Associated with Posttraumatic Stress Disorder Following Moderate to Severe Traumatic Brain Injury: A Prospective Study. Depression and Anxiety, 33(1), 19–26.
https://www.ptsd.va.gov/publications/rq_docs/V30N2.pdf
Bathina, S., Undurti, N. D., (2015) Brain-derived neurotrophic factor and its clinical implications,
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4697050/
Bergersen, K., Halvorsen, J. Ø., Tryti, E. A., Taylor, S. I., & Olsen, A. (2017). A systematic literature review of psychotherapeutic treatment of prolonged symptoms after mild traumatic brain injury. Brain Injury, 31(3), 279–289.
https://doi.org/10.1080/02699052.2016.1255779
Bomyea, J., Flashman, L. A., Zafonte, R., Andaluz, N., Coimbra, R., George, M. S., … Stein, M. B. (2019). Associations between neuropsychiatric and health status outcomes in individuals with probable mTBI. Psychiatry Research, 272, 531–539.
https://www.ncbi.nlm.nih.gov/pubmed/30616120
Caldieraro, M. A., & Cassano, P. (2019). Chapter 35—Transcranial photo-biomodulation for major depressive and anxiety disorders and for posttraumatic stress disorder. In M. R. Hamblin & Y.-Y. Huang (Eds.), Photo-biomodulation in the Brain (pp. 479–487).
https://doi.org/10.1016/B978-0-12-815305-5.00035-X1
Casler, M., Fosmire,A., Klein, D., (2019) Support for Veterans: Community Reintegration, Family and Mental Health Needs – ProQuest.
https://search.proquest.com/openview/d9017c9dd1fa574fab507fb3cdcda737/1?pqorigsite=gscholar&cbl=18750&diss=y
Chao, L. L. (2019). Improvements in Gulf War Illness Symptoms After Near-Infrared Transcranial and Intranasal Photo-biomodulation: Two Case Reports. Military Medicine.
https://doi.org/10.1093/milmed/usz037
Cushman, J. H., (2012, February 24). New Study Gives Scope and Cost of Combat-Related Conditions Among Veterans. At War B
https://atwar.blogs.nytimes.com/2012/02/24/new-study-gives-scope-and-cost-of-combatrelated-conditions-among-veterans/
Dismuke-Greer, C. E., Gebregziabher, M., Byers, A. L., Taber, D., Axon, N., Yaffe, K., & Egede, L. E. (2019). Comorbid TBI-depression costs in veterans: A chronic effect of neurotrauma consortium (CENC) study. Brain Injury, 33(2), 198–204.
https://doi.org/10.1080/02699052.2018.1542508
DoD Worldwide Numbers for TBI. (2018). DVBIC website: https://dvbic.dcoe.mil/dodworldwide-numbers-tbi
Donald, C. L. M., Barber, J., Patterson, J., Johnson, A. M., Dikmen, S., Fann, J. R., & Temkin, N. (2019). Association Between 5-Year Clinical Outcome in Patients With Nonmedically Evacuated Mild Blast Traumatic Brain Injury and Clinical Measures Collected Within 7 Days Postinjury in Combat. JAMA Network Open, 2(1), e186676–e186676.
https://doi.org/10.1001/jamanetworkopen.2018.6676
Eapen, B. C., & Subbarao, B. (2019). Traumatic Brain Injury. In E. C. Ritchie & M. D. Llorente (Eds.), Veteran Psychiatry in the US: Optimizing Clinical Outcomes (pp. 211–231).
https://doi.org/10.1007/978-3-030-05384-0_14
Elder, G. A., Ehrlich, M. E., & Gandy, S. (2019). Relationship of traumatic brain injury to chronic mental health problems and dementia in military veterans. Neuroscience Letters, 707, 134294.
https://doi.org/10.1016/j.neulet.2019.134294
Fox, S., & Campbell, V. (2019). Chapter 24 – Effects of photo-biomodulation on traumatic brain injury: Proposed clinical assessment. In M. R. Hamblin & Y.-Y. Huang (Eds.), Photobiomodulation in the Brain (pp. 299–307). https://doi.org/10.1016/B978-0-12-815305-5.00024-5″815305-5.00024-5
Fish, L., & Scharre, P. (2018). Protecting Warfighters from Blast Injury. 24. Frick, K. D., & Singman, E. L. (2019). Cost of Military Eye Injury and Vision Impairment Related to Traumatic Brain Injury: 2001–2017. Military Medicine, 184(5–6), e338–e343.
https://doi.org/10.1093/milmed/usy420
Hamblin, M. R. (2019). Chapter 8—Mechanisms of photo-biomodulation in the brain. In M. R. Hamblin & Y.-Y. Huang (Eds.), Photo-biomodulation in the Brain (pp. 97–110).
https://doi.org/10.1016/B978-0-12-815305-5.00008-7
Hayes, J. P. (2019). PTSD and TBI Comorbidity. 30(2), 18.
https://www.ptsd.va.gov/publications/rq_docs/V30N2.pdf
Hisle-Gorman, E., Susi, A., & Gorman, G. H. (2019). The Impact Of Military Parents’ Injuries On The Health And Well-Being Of Their Children. Health Affairs, 38(8), 1358–1365.
https://doi.org/10.1377/hlthaff.2019.00276
Huang, Y.-Y., & Hamblin, M. R. (2019). Chapter 4—Photo-biomodulation on cultured cortical neurons. In M. R. Hamblin & Y.-Y. Huang (Eds.), Photo-biomodulation in the Brain (pp. 35–47).
https://doi.org/10.1016/B978-0-12-815305-5.00004-X
Kaplan, G. B., Leite-Morris, K. A., Wang, L., Rumbika, K. K., Heinrichs, S. C., Zeng, X., …Teng, Y. D. (2017). Pathophysiological Bases of Comorbidity: Traumatic Brain Injury and Post-Traumatic Stress Disorder. Journal of Neurotrauma, 35(2), 210–225.
https://doi.org/10.1089/neu.2016.4953
Kempuraj, D., Ahmed, M. E., Selvakumar, G. P., Thangavel, R., Dhaliwal, A. S., Dubova, I., … Zaheer, A. (2019). Brain Injury–Mediated Neuro-inflammatory Response and Alzheimer’s Disease. The Neuroscientist, 1073858419848293.
https://doi.org/10.1177/1073858419848293
Kontos, A. P., Kotwal, R. S., Elbin, R. j., Lutz, R. H., Forsten, R. D., Benson, P. J., & Guskiewicz, K. M. (2012). Residual Effects of Combat-Related Mild Traumatic Brain Injury. Journal of Neurotrauma, 30(8), 680–686.
https://doi.org/10.1089/neu.2012.2506
Kulkarni, P., Morrison, T. R., Cai, X., Iriah, S., Simon, N., Sabrick, J., … Ferris, C. F. (2019). Neuroradiological Changes Following Single or Repetitive Mild TBI. Frontiers in Systems Neuroscience, 13, 34.
https://doi.org/10.3389/fnsys.2019.00034
Ling, G., Bandak, F., Armonda, R., Grant, G., & Ecklund, J. (2009). Explosive Blast Neurotrauma. Journal of Neurotrauma, 26(6), 815–825.
https://doi.org/10.1089/neu.2007.0484
Lindenfeld, G., Rozelle, G., Soutar, R., Hummer, J, & Sutherland, M. (2019a) Post-traumatic stress remediated: A study of eight combat veterans. New Mind Journal (www.nmindjournal.com).
Lindenfeld, G., Rozelle, G., Soutar, R., Hummer, J, & Sutherland, M. (2019b). Remediation of PTSD in a Combat Veteran: A Case Study. NeuroRegulation, 6(2), 102–102.
https://doi.org/10.15540/nr.6.2.102
Lindenfeld, G. L., & Rozelle, G. (2019c). Chapter 37 – Signature wounds of war: A case study. In M. R. Hamblin & Y.-Y. Huang (Eds.), Photo-biomodulation in the Brain (pp. 503–514).
https://doi.org/10.1016/B978-0-12-815305-5.00037-3
Lindenfeld, G., Zumwalt, T., Hummer, J., Billiot, K., Rozelle, G., (2019d) When ‘Thank You for Your Service’ Is No Longer Enough: Special Forces, Resilience & Suicide, Manuscript submitted for publication.
Lipton, B., The Wisdom of Your Cells. (2012).
https://www.brucelipton.com/resource/article/the-isdom-your-cells
Mohamed, A. Z., Cumming, P., Götz, J., Nasrallah, F., & for the Department of Defense Alzheimer’s Disease Neuroimaging Initiative. (2019). Tauopathy in veterans with longterm posttraumatic stress disorder and traumatic brain injury. European Journal of Nuclear Medicine and Molecular Imaging, 46(5), 1139–1151.
https://doi.org/10.1007/s00259-018-4241-7
Naeser, M. A., Martin, P. I., Ho, M. D., Krengel, M. H., Bogdanova, Y., Knight, J. A., … Koo, B.-B. (2019). Chapter 25 – Transcranial, red/near-infrared light-emitting diode therapy for chronic traumatic brain injury and poststroke aphasia: Clinical studies. In M. R. Hamblin & Y.-Y. Huang (Eds.), Photo-biomodulation in the Brain (pp. 309–331).
https://doi.org/10.1016/B978-0-12-815305-5.00025-7
Peskind, E. R., Petrie, E. C., Cross, D. J., Pagulayan, K., McCraw, K., Hoff, D., … Minoshima, S. (2011). Cerebrocerebellar Hypometabolism Associated With Repetitive Blast Exposure Mild Traumatic Brain Injury in 12 Iraq War Veterans With Persistent Post-Concussive Symptoms. Neuroimage, 54(Suppl 1), S76–S82.
https://doi.org/10.1016/j.neuroimage.2010.04.008
Ponsford, J. L., Downing, M. G., Olver, J., Ponsford, M., Acher, R., Carty, M., & Spitz, G. (2014). Longitudinal Follow-Up of Patients with Traumatic Brain Injury: Outcome at Two, Five, and Ten Years Post-Injury. Journal of Neurotrauma, 31(1), 64–77.
https://doi.org/10.1089/neu.2013.2997
Pugh, M. J., Swan, A. A., Carlson, K. F., Jaramillo, C. A., Eapen, B. C., Dillahunt-Aspillaga, C.,… Grafman, J. H. (2018). Traumatic Brain Injury Severity, Comorbidity, Social Support, Family Functioning, and Community Reintegration Among Veterans of the Afghanistan and Iraq Wars. Archives of Physical Medicine and Rehabilitation, 99(2, Supplement), S40–S49.
https://doi.org/10.1016/j.apmr.2017.05.021
Romeu-Mejia, R., Giza, C. C., & Goldman, J. T. (2019). Concussion Pathophysiology and Injury Biomechanics. Current Reviews in Musculoskeletal Medicine, 12(2), 105–116.
https://doi.org/10.1007/s12178-019-09536-8
Salehpour, F., Hamblin, M. R., & DiDuro, J. O. (2019). Rapid Reversal of Cognitive Decline, Olfactory Dysfunction, and Quality of Life Using Multi-Modality Photo-biomodulation Therapy: Case Report. Photo-biomodulation, Photomedicine, and Laser Surgery, 37(3), 159–167.
https://doi.org/10.1089/photob.2018.4569
Santhanam, P., Wilson, S. H., Oakes, T. R., & Weaver, L. K. (2019). Effects of mild traumatic brain injury and post-traumatic stress disorder on resting-state default mode network connectivity. Brain Research, 1711, 77–82.
https://doi.org/10.1016/j.brainres.2019.01.015
Stocker, R. P. J., Cieply, M. A., Paul, B., Khan, H., Henry, L., Kontos, A. P., & Germain, A. (2014). Combat-related blast exposure and traumatic brain injury influence brain glucose metabolism during REM sleep in military veterans. NeuroImage, 99, 207–214.
https://doi.org/10.1016/j.neuroimage.2014.05.067
Taylor, B. C., Hagel, E. M., Carlson, K. F., Cifu, D. X., Cutting, A., Bidelspach, D. E., & Sayer, N. A. (2012). Prevalence and Costs of Co-occurring Traumatic Brain Injury With and Without Psychiatric Disturbance and Pain Among Afghanistan and Iraq War Veteran VA Users. Medical Care, 50(4), 342–346.
https://www.jstor.org/stable/23216628?seq=1#page_scan_tab_contents
Thakur, H., Oni, O., Singh, V., Sharma, R., Sharma, M., Maalouf, S., … Oehlert, M. (2018). Increases in the Service Connection Disability and Treatment Costs Associated With Posttraumatic Stress Disorder and/or Traumatic Brain Injury in United States Veterans Pre- and Post-9/11: The Strong Need for a Novel Therapeutic Approach. Epidemiology: Open Access, 08(04).
https://doi.org/10.4172/2161-1165.1000353
Traumatic Brain Injury | Concussion | Traumatic Brain Injury | CDC Injury Center. (2019, July 11).
https://www.cdc.gov/traumaticbraininjury/index.html
Voris, S. E., & Steinkopf, J. (2019). Suffering in the Shadows: Interviews with Wives of Combat Veterans Suffering from Post-Traumatic Stress Disorder and/or Traumatic Brain Injury. Marriage & Family Review, 55(6), 493–511.
https://doi.org/10.1080/01494929.2018.1519494
Zomorrodi, R., Loheswaran, G., Pushparaj, A., & Lim, L. (2019). Pulsed Near Infrared Transcranial and Intranasal Photo-biomodulation Significantly Modulates Neural Oscillations: A pilot exploratory study. Scientific Reports, 9(1), 1–11.
https://doi.org/10.1038/s41598-019-42693-x