Alpha Dominant Frequency & Depression: Findings 3
Richard Soutar, Ph.D. BCN
What role does physiology play in depression as reflected in the Interactive Self Inventory ISI? As depression scores increase in the Depression measure on the ISI, what changes in physiology and electrophysiology occur as measured by the Physiology Checklist and the qEEG? Based on my paper qEEG and Oxidative Stress (Soutar, 2018), excessive excitotoxicity due to chronic distress increases glutamate output and the production of high levels of free radicals. This triggers a pro-inflammatory response which in turn redirects 5HTP from serotonin production toward quinolinic acid production. This in turn tends to reduce ATP output and diminishes cortical high frequency or beta activity. The brain in response drifts progressively toward an idling mode with enhanced alpha output which tends to be greater in the left hemisphere than the right.
At the same time as alpha amplitude increases, there often is a diminishing cortisol output in response to chronic adrenal output in an effort by the body to conserve resources and general physiological system fatigue. This is predicted by Selye’s model of stress. Thyroid activity is altered as well in response to chronic physiological hyperarousal and Thyroid T3 deficits tend to emerge (Scicutella, 2007). Neuronal T3 transport mechanisms also diminish which may further reduce ATP production as well.
Between the inflammatory activity, serotonin production deficits and diminished T3, a general slowing should be expected in the alpha frequency bands. These changes significantly burden the brain’s energy production capacity. This alpha slowing tends to contribute to increased alpha amplitude as well due to the fundamental dynamics of energy production in the brain (Nunez and Srinivason, 2006). Clinical observation and client reports often include high levels of mental chatter. The relationship between high levels of cortical alpha related to mental chatter has been noted by Ros et al (2013) and correlates to posterior high amplitude alpha activity with reduced MRI activity. The New Mind map system often locates this anxiety related alpha as being especially predominant in the posterior cingulate region around P3-Pz-P4 as well. It tends to dominant in the left hemisphere with increased depressive symptom reports as noted in Findings 1.
The key characteristic of the mental chatter is related to a busy mind preoccupied with tasks to be completed and managing behavior details with respect to controlling environmental and social factors. This activity has been previously defined as Perfectionism in Findings 2. The more significant the depression reports on the ISI, the higher the eyes open alpha amplitude appears to be. Often this can be in the 25uv-35uv range or higher. Failure to perform well leads to a sense of a loss of control due to social inaccuracy and aggravates competitive tendencies resulting in growing frustration and hopelessness. The overall expectation is that excessive cortical activity eventually exhausts the brain and in turn diminishes the brains activity to routine and stereotypical mental chatter, less demanding on cortical resources than active exploratory problem solving efforts and worry. This perseverant activity appears to particularly impact the posterior cingulate and its attention related activity and there-by diminishing attentional release of stimuli of interest (Peterson & Posner, 2012). The result should be slowed high amplitude alpha that progressively tends to drift into left hemisphere dominance. This agrees with our New Mind spectrum theory of anxiety-depression.
The mean score for physiological symptoms of clinical clients is 78 in the New Mind assessment system. Based on the ACE study (Shonkoff & Garner, 2012), those with a history of toxic stress should progressively exhibit both higher physiological symptom scores and higher anxiety and depression symptom scores over time. In addition, the research on the relationship between the Microbiome and depression (O’Mahoney, 2015) indicates that the inflammatory process in the brain and in the GI tract are bi-directional and mediated by white blood cell signaling in both regions.
To test this hypothesis, we selected a group of clinical adults from the New Mind Database (N=751) and compared those with low scores on physiological symptoms to those with high score on physiological symptoms. The depression scores for those scoring below the Physio mean score of 78 were 13.3 (n= 674) and in the low subclinical range. The depression scores for those with High Physio scores was 20.1 (n=77) , which is in the low to moderate clinical range. These results are supportive of the ACE study and the New Mind Oxidative Stress Model of qEEG. Chronic anxiety and depression typically are associated with chronic health problems and likely major contributors.
Based on the preceding analyses, alpha frequency slowing and elevated alpha amplitude would be expected to also be found associated with these conditions. In an attempt to support and confirm these expectations based on the literature, samples were drawn from the New Mind Database for further analyses.
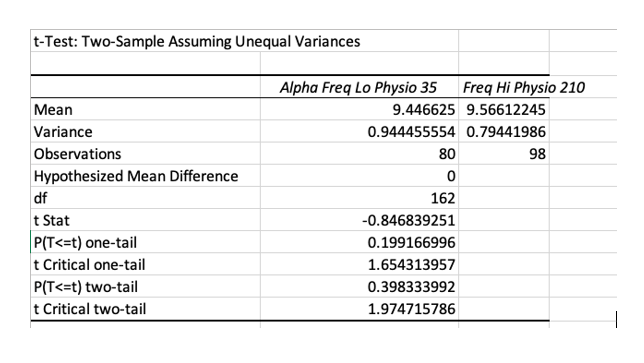
In comparing those with very low physiological scores of less than 35 with those with very high physio score greater than 210, it was found that there was no significant difference in alpha frequency between the two groups N = 178). So having a lot of physiological problems alone does not necessarily result in slowed alpha. Slowing may be more specifically related to a particular issue such as Thyroid or Liver issues as reported by Neidermeyer & Lopes da Silva (2005).
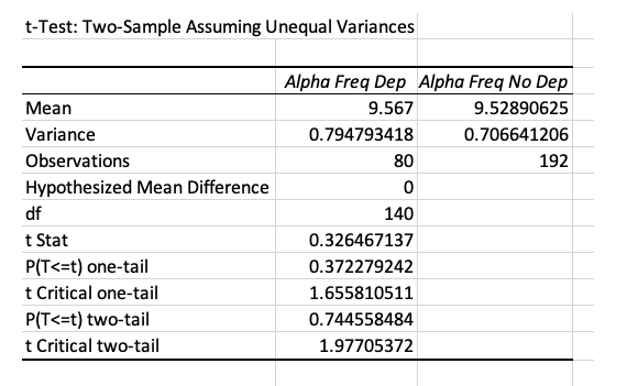
Looking at the relationship between depression and slowed alpha alone we find a similar unexpected pattern. Psychological depression may involve less slowing of the EEG than thyroid conditions or other health problems.
A great amount of physical health problems alone or significant depression alone may not always affect alpha dominant frequency. What about the two together? Do those with high physio scores and high depression scores have lower frequency alpha. In looking at 131 cases at Cz with both high scores in Physiological problems and High scores in depression, 63 cases had scores lower than 9.5Hz. The mean frequency for this group was 9.6Hz. There were 24 cases with dominant frequency greater than 10.5Hz. Only 45 cases were in normal range. Comparing those in normal frequency range with those outside the norm, only 34% were in normal frequency range. So it is at least more common to find abnormal dominant frequency in those who are depressed and in poor health than to find normal dominant frequency, but it is not always lower than normal. This suggests again that there may be specific problems that are associated with high or low dominant frequency such as thyroid or liver function related to slowed alpha as mentioned above or insulin sensitivity related to fast alpha.
Using 2019 Cz New Mind data, ISI depression scores are significantly higher in those with high amplitude alpha (>18Uv) that is also Low in frequency (< 9.5) than depression scores in those with normal amplitude alpha (< 18uv) that is in normal frequency range (9.5-10.5 Hz). Using a one tail test in the positive direction. The effect size is small however, suggesting other variables are in play.
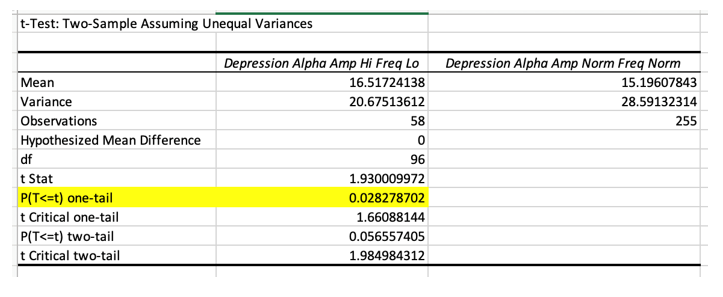
In sum the idea that depression is related to high amplitude low frequency alpha as well as poor physiological symptoms seems to be valid but weak and alpha dominant frequency does not predict depression or physiological problems by itself. Other important factors apparently play a role.
References
Niedermeyer, E., Lopes da Silva, F.H. (2005). Electroencephalography: Basic principles, clinical applications, and related fields. Lippincott Williams & Wilkins: New York.
Nunez, Paul L., Srinivasan, Ramesh (2006). Electric fields of the brain: The neurophysics of EEG. New York: Oxford University Press. (Second Edition).
O’Mahoney, S. M., Clark, G., Borre, Y. E., Dinan, T. G., Crvan, J. F. (2015). Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behavior Brain Research, 277:32-48. doi: 10.1016/j.bbr.2014.07.027.
Peterson, S., Posner, M (2012). The attention system of the brain: 20 years after. Annu. Rev. Neurosci, 35, 73–89. DOI: 10.1146/annurev-neuro-062111-150525
Ros, T., Théberge, J., Frewen, P. A., Kluetsch, R., Densmore, M., Calhoun, V. D., & Lanius, R. A. (2013). Mind over chatter: plastic up-regulation of the fMRI salience network directly after EEG neurofeedback. NeuroImage, 65, 324–335. https://doi.org/10.1016/j.neuroimage.2012.09.046
Scicutella, Angela (2007). Neuropsychiatry and traumatic brain injury. In Jean Elbaum & Deborah M. Benson. (Eds.) Acquired brain injury: An integrative neuro-rehabilitation approach (pp81-121). New York: Springer.